 My apologies for the lateness of this post! It was a hospital day yesterday and afterwards my wonderful husband surprised me with an impromptu date night, and we got in late. Also actual writing had to happen and I wasn’t sure what to say, but finally, here we go.
My apologies for the lateness of this post! It was a hospital day yesterday and afterwards my wonderful husband surprised me with an impromptu date night, and we got in late. Also actual writing had to happen and I wasn’t sure what to say, but finally, here we go.
 The theme for Week 3 in the Meditation Series is gathering the scattered mind. I’ll be honest that lately I have been incredibly scattered because I have been waiting for scan results, so this weeks practice has been pretty spotty and I’ve been so easily distracted.
The theme for Week 3 in the Meditation Series is gathering the scattered mind. I’ll be honest that lately I have been incredibly scattered because I have been waiting for scan results, so this weeks practice has been pretty spotty and I’ve been so easily distracted.
For the last little while, I have been learning to live with results that don’t quite meet up with my expectations. It isn’t that they ‘re bad results, its just not the results I want. For a very long time, I was blessed after a course of scans to get the wonderful news that I was NED (No Evidence of Disease), but since I progressed last year and changed meds, I haven’t quite gotten there.
Overall, I am very healthy and all the results show that I am stable. The results say my brain and organs are unremarkable (good news ironically) because it means that the cancer is still only in my lungs. The problem lies in the lungs. Although things have not changed from previous studies, within the results, there have always been comments about “stable globular masses” or “stable pleural effusions” and frankly I hate knowing that there is cancer is living in me and that my lungs are trying desperately to kill me.
I don’t know if I was under the misguided impression that NED meant that the cancer was gone or dormant, but it certainly gave me a sense of security and comfort, and not having it keeps me on edge. After all, there is no uncertainty that there is or isn’t cancer in me, its in here and its trying very hard to be active.
As hard as I try not to fixate or catastrophize, I can’t reconcile those feelings of insecurity and chaos when I know how precariously balanced I am on the edge.
Maybe its all in the wording
Words.
Never say words don’t matter.
Words have power.
In my case they have the power to set my mind spinning down a trajectory of sadness and fear, which is why I’m really glad that I am posting this MBSR series, because it forces me to recognize these anxieties.
Perhaps as you have been practicing your meditations, you have found yourself wandering too?
Now that we have been practicing for a couple of weeks, you might actually be noticing how busy your mind can be. I know mine certainly is!! You may be replaying past events or have expectations of the meditation, or be noticing fearful thoughts, or even running through your grocery list of chores. Its ok.
You might even be feeling frustrated that you can’t “clear” your mind of those thoughts, or that your mind is wandering. That’s ok. The kind of meditation that we are learning with MBSR isn’t about getting rid of our thoughts and distractions. Its learning to recognize them. Its human nature to want to strive for something or achieve a goal, but here the goal is to have no goals.
I know it sounds a little nuts, but really its such a useful skill. One of the reasons I think the MBSR program is so intense, is to help us to slow down, be deliberate, and to make the skills learned part of our daily routines.
This week we will introduce a new type of meditation. Mindful movement. The idea being that by being more aware of our physical and mental state, we are allowed to be more present in the here and now. These movements encourage us to take time to pause by bringing our attention totally into the body and try to marry our breath with our movements.
Remember though, the goal here is not to have goal. Try to resist the temptation of say having the goal of relaxation. Relaxation might happen, in which case that’s great, but maybe it doesn’t in which case that’s great too, because maybe you noticed that you were carrying tension in your neck and shoulders, which leads you to notice that you are holding on to a negative event that happened earlier on in the day. Then maybe as a result of that noticing, you realize that you had been tense over a non-event and decide to let it go. That’s what can happen when we start recognize our thoughts and our body sensations.
So with that, we introduce Mindful Walking, and Hatha Yoga. I’ll break them down and link to some videos that can help with home practice below. In addition, if you practice Qigong or Tai-Chi these can also act as mindful movements.
Before I post the new practices and homework, I want to hear from you.
How have you been finding things? How did you like last weeks practice? What were some of the pleasant events you experienced? If you want to share, I encourage you to leave me a comment. If you’d like me to share it, let me know too, or else I’ll keep them private.
Be well and happy practice.
AM
Activities for Week I can be found here, and for Week 2 here.
Activity I: Unpleasant Events
Last week we had the opportunity to become aware of thoughts and feeling we felt when we experienced pleasant events, this week, we are going to focus on unpleasant events. The activity will act the same as last week where you will notice and record events (for yourself) in a chart or journal.
| Day | What was the experience? | How did your body feel, in detail during this experience? | What moods and feelings accompanied this experience? | What thoughts went through your mind? | What thoughts are in your mind as you write this down? |
| Example | I found a parking ticket on my car. | My shoulders got tense and raised, my forehead became tense, my stomach became upset. | Frustration, anger, irritation | “I was sure I could park there.” “What a waste of money!” | “Ugh I hate parking tickets”
|
Meditation I: Seated Mindful Breathing
Practice mindful breathing seated in a chair or on the floor, make sure you are sitting so that your spine is self-supporting. If seated on the floor, do so on a firm, thick cushion (or a pillow folded over once or twice). Whatever you sit on, make sure your hips are slightly higher than your knees.
Meditation 2: The 3-Minute Breathing Space
Step 1- Becoming Aware – You can do this sitting or standing. If possible, close your eyes. Then bring your awareness to your inner self by asking yourself, “What is my experience right now?”
- What thoughts are going through my mind? (As best as you can, acknowledge thoughts as mental events, try to put them into words.)
- What feelings are here? (Turn toward any sense of discomfort or unpleasant feelings, acknowledging them.)
- What body sensations are here right now? (Quickly scan your body to pick up any sensations of tightness or tension, acknowledge them.)
Step 2 – Gathering – Redirect your attention from physical body sensations to sensations of your breath and breathing itself. Feel your abdomen expanding and contracting. Expansion as you breathe in and contraction as it goes out. Follow your breath all the way in and all the way out, using your breath as an anchor.
Step 3 – Expanding – Try to expand the field of your awareness from your abdomen to include your whole body. Imagine your entire body inhaling and exhaling. Try to notice your posture and facial expressions or if you note any sensations of discomfort, tension, resistance and bring your awareness to those sensations by breathing into them.
Meditation 3: Mindful Walking
This can be done inside at home, or out in the real world. The key here is to be deliberate and attentive.
- Stand straight and tall but not stiff. Take a moment to feel your feet on the ground and let your weight be distributed evenly. Are you leaning to one side or the other, or on your toes or heels?
- Your hands can be folded gently at your abdomen, or if you are more comfortable just by your sides naturally.
- Drop your gaze slightly.
- Step out with the left foot. Feel it swing out. Feel the way your heel strikes the ground, then the ball of the foot and finally the toes. How has your balance changed?
- Feel how your body moves as your right foot steps forward. Feel the heel hit the ground, then the ball of the foot, and finally the toes.
- Walk at a steady pace, one that is slightly slower than you would walk normally.
Your first few steps may be awkward as you are trying to notice all those sensations that we normally do automatically. Once you have done this a few times, you won’t look like a zombie. So maybe the first time you try this, you may want to be at home or in your own yard.
Handy Tips:
- Flat space
- Barefoot (If you like)
- Be slow and attentive
- Try to focus on feeling the sensations of stretching and bending, change of balance and weight as your body as it moves.
- Try to feel the pull of gravity and the groundedness of moving through your feet (heel….pads….toes).
Meditation 4: Yoga
There are many kinds of yoga and all are based on basic poses or asanas, but we will focus on Hatha yoga which marries poses (Asanas) with breath or Pranayama. Hatha yoga helps prepare the body and mind for other meditation practices. It is relatively gentle, slow and great for beginners. *
*If you have any health concerns or conditions, please consult with your physician before starting the movement portion.
Home Work:
- Everyday: Practice using the 3-Minute Breathing Space, three times or at least once daily at pre-determined time. (I love this one, and use it all the time!) In addition complete the Unpleasant Events Journal.
- On days 1, 3, and 5 practice Mindful Walking and record your experience and observations in your home practice journal.
- On days 2, 4, and 6 practice Hatha Yoga and record your experience and observations in your home practice journal.
Meditations:
Body Scan and Mindful Breathing (optional)
New Resources:
Mindful Magazine – Nice site that has tons of great articles and meditations.



 Mindful Breathing is another tool that helps us to ground us and bring gentle awareness to ourselves without judgment or need to change anything about our situation. We simply breathe and notice our body as we do so. I tend to have a challenge doing this one on my own and need to listen to a guided meditation. I find I am able to focus on my breath with more attention having someone guide me than if I did this on my own. Its ok if your mind wanders while you practice, it is completely normal and expected. So don’t judge or think you failed. Just notice the thoughts or the fact that you have wandered, and refocus on your breath. If it happens again (and it probably will) just acknowledge and refocus. That’s the beauty of breathing; every breath is a new opportunity to start again.
Mindful Breathing is another tool that helps us to ground us and bring gentle awareness to ourselves without judgment or need to change anything about our situation. We simply breathe and notice our body as we do so. I tend to have a challenge doing this one on my own and need to listen to a guided meditation. I find I am able to focus on my breath with more attention having someone guide me than if I did this on my own. Its ok if your mind wanders while you practice, it is completely normal and expected. So don’t judge or think you failed. Just notice the thoughts or the fact that you have wandered, and refocus on your breath. If it happens again (and it probably will) just acknowledge and refocus. That’s the beauty of breathing; every breath is a new opportunity to start again.


 though, life began infiltrating these moments and I found myself falling back into old habits. I found myself complaining about the weather (as Canadians will do), feeling my blood boil when I was stuck in traffic, the stars were dimmer, and then I stopped noticing.
though, life began infiltrating these moments and I found myself falling back into old habits. I found myself complaining about the weather (as Canadians will do), feeling my blood boil when I was stuck in traffic, the stars were dimmer, and then I stopped noticing.
 It isn’t for the feint of heart, because of the time commitment (8 Weeks + home practice), but I swear it is worth it. Each week I would meet with a small group of stressed out over worked harried individuals and we would learn a specific practice or a few. Then we were tasked with homework. Typically it was an exercise in attention, some sort of meditation, and a very short “journal”. Initially it was a challenge fitting it in, but somehow if you are committed, you do find time.
It isn’t for the feint of heart, because of the time commitment (8 Weeks + home practice), but I swear it is worth it. Each week I would meet with a small group of stressed out over worked harried individuals and we would learn a specific practice or a few. Then we were tasked with homework. Typically it was an exercise in attention, some sort of meditation, and a very short “journal”. Initially it was a challenge fitting it in, but somehow if you are committed, you do find time.


 to her wit and humour. Carrie’s Leia was the first princess I ever wanted to be. I mean why not? She was plucky, beautiful, spunky and carried a blaster, what little girl wouldn’t want to be her?! Sadly I was ill equipped and lacked the follicular capacity to create those famous cinnamon buns, Cinderella it was. All humour aside, her passing reminded me that all of us struggle, sometimes it is invisible and private and sometimes it is right there in your face. Regardless of which it is, we all have the capacity and grace to pull ourselves up and make a comeback.
to her wit and humour. Carrie’s Leia was the first princess I ever wanted to be. I mean why not? She was plucky, beautiful, spunky and carried a blaster, what little girl wouldn’t want to be her?! Sadly I was ill equipped and lacked the follicular capacity to create those famous cinnamon buns, Cinderella it was. All humour aside, her passing reminded me that all of us struggle, sometimes it is invisible and private and sometimes it is right there in your face. Regardless of which it is, we all have the capacity and grace to pull ourselves up and make a comeback. had an inkling that it may come around again post Dx and tried to head it off at the pass, but your body and mind have a way of telling you it needs help.
had an inkling that it may come around again post Dx and tried to head it off at the pass, but your body and mind have a way of telling you it needs help.


 done on metastatic patients, or patients who are outliers? I imagine they feel neglected too. In the U.S., part of this problem may have just been addressed with the signing of the 21st Centuries Cures Act. The rest of the world however may not have a course correction, so we need to be able to recognize that in order to have equality, we need to point out the inequities. Then instead of cutting the pie smaller, we need to bake a bigger pie. We need to break down barriers, and share information. More and more we see that the driving mutations in different disease groups are the same.
done on metastatic patients, or patients who are outliers? I imagine they feel neglected too. In the U.S., part of this problem may have just been addressed with the signing of the 21st Centuries Cures Act. The rest of the world however may not have a course correction, so we need to be able to recognize that in order to have equality, we need to point out the inequities. Then instead of cutting the pie smaller, we need to bake a bigger pie. We need to break down barriers, and share information. More and more we see that the driving mutations in different disease groups are the same.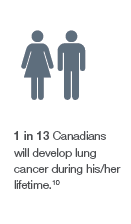 Every year 28,4001 Canadians and 221,2002 Americans are diagnosed with lung cancer. Of those diagnosed, 20,8003 in Canada and 157,4994 in the US will have their lives taken from this disease. The truth is that while many other cancers have improved 5-year survival rates, lung cancer still remains one of the lowest at about 17%5.
Every year 28,4001 Canadians and 221,2002 Americans are diagnosed with lung cancer. Of those diagnosed, 20,8003 in Canada and 157,4994 in the US will have their lives taken from this disease. The truth is that while many other cancers have improved 5-year survival rates, lung cancer still remains one of the lowest at about 17%5. If one has asked me what type of cancer I thought I may get in my lifetime, seven years ago before lung cancer happened to me, I would have thought it would be breast cancer. After all, I am a woman with breasts and like many, I didn’t think that because I was human and had lungs that I’d be at risk. The reality is, one of the fastest growing segments in lung cancer is the population of young, non/never smokers (17.9%)7. Add to that the population of people who had previously quit smoking (60%)8, and you begin to get a different picture of lung cancer.
If one has asked me what type of cancer I thought I may get in my lifetime, seven years ago before lung cancer happened to me, I would have thought it would be breast cancer. After all, I am a woman with breasts and like many, I didn’t think that because I was human and had lungs that I’d be at risk. The reality is, one of the fastest growing segments in lung cancer is the population of young, non/never smokers (17.9%)7. Add to that the population of people who had previously quit smoking (60%)8, and you begin to get a different picture of lung cancer.

You must be logged in to post a comment.